Learn how physical therapy can help with Parkinson’s disease from our physical therapist Jennifer Deskiewicz. Watch the video or read the transcript below.
 Hi, everyone. I’m Jen Deskiewicz. I’m a physical therapist here at Carroll Lutheran Village in the outpatient department. I’ve been here for 18 years and have been a therapist for about 24 years. I’m going to share with you today about managing Parkinson’s disease and the role we can help play in it, as physical therapists.
Hi, everyone. I’m Jen Deskiewicz. I’m a physical therapist here at Carroll Lutheran Village in the outpatient department. I’ve been here for 18 years and have been a therapist for about 24 years. I’m going to share with you today about managing Parkinson’s disease and the role we can help play in it, as physical therapists.
Briefly, Parkinson’s is a disease that affects the central nervous system. What happens is nerve cells start to die. When that dying occurs, dopamine, which is the chemical messenger that comes from the brain and goes to the muscles for muscle control and coordination, becomes greatly affected.
Parkinson’s is a chronic and progressive disorder. It continues to worsen over time. Many people live with active Parkinson’s and have an active lifestyle for many years, even in excess of 20 years. We’re seeing Parkinson’s onset at a younger age. Many of you are familiar with Michael J. Fox who was diagnosed in his 40’s.
There are ways to manage and cope and still have a healthy lifestyle and try to slow down the process of Parkinson’s. It is very important to receive a proper diagnosis. You really should see a neurologist. A movement specialist can help with this process as well. It’s very important to become well informed in the beginning. That way you can have a good plan in place with your primary care doctor, neurologist and physical therapy team.
There are medicines that can help with replacing dopamine loss. Those medications combined with coordination with physical therapy can be very beneficial for Parkinson’s.
What do we see with Parkinson’s Disease?
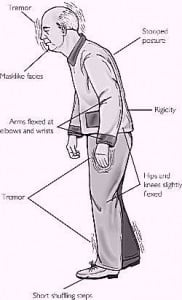
- Increased muscle stiffness and rigidity
- Postural changes, especially in the later stages of Parkinson’s
- Rigidity through the core, leg muscles and arms
 The postural changes that tend to happen overtime with the normal aging process become even greater with Parkinson’s. We see muscle strength decrease if we’re not moving as much. You’ve likely heard the old adage, “if you don’t use it, you lose it.” If we’re not moving around, especially as Parkinson’s continues to progress, we’re going to have decreased muscle strength. This will affect how we are able to move throughout the day, our gait (the way we walk) and function.
The postural changes that tend to happen overtime with the normal aging process become even greater with Parkinson’s. We see muscle strength decrease if we’re not moving as much. You’ve likely heard the old adage, “if you don’t use it, you lose it.” If we’re not moving around, especially as Parkinson’s continues to progress, we’re going to have decreased muscle strength. This will affect how we are able to move throughout the day, our gait (the way we walk) and function.
Some early symptoms we may see are tremors or involuntary shaking movements. I want to emphasize there are other issues related with tremors. Just because you might have a slight tremor does not automatically mean you have Parkinson’s. It is very important to get a proper diagnosis.
 Some patients have resting tremors, where they are shaking even in a resting mode, and that does not mean that they have Parkinson’s. I don’t want someone to hear some of these signs and think all of a sudden, “oh, I have Parkinson’s.”
Some patients have resting tremors, where they are shaking even in a resting mode, and that does not mean that they have Parkinson’s. I don’t want someone to hear some of these signs and think all of a sudden, “oh, I have Parkinson’s.”
Other early symptoms include:
- Masked facial expressions, caused by a decrease in muscle tone and control
- Slowed and softer speech – a lot of times spouses will say their loved one is just not speaking loud enough. This results from the throat muscles weakening. Additionally, if the muscles are atrophying and not being used as much, the signal to those muscles decreases and the voice changes, becoming slower and softer. In physical therapy, we have speech therapists who can work with these changes and help provide a solution, which may include working on projecting and speech cadence. There are a lot of different exercises we can offer on a rehab basis for Parkinson’s with speech difficulties. Weakening throat muscles can also decrease swallowing ability and may increase the likelihood of choking and drooling. These are things that are affected by Parkinson’s and certainly can increase and worsen as the stages progress.
- Decrease in the gait (i.e. the way we walk) – you might see a shuffling or freezing when you walk; this is occurs into the middle and later stages. Change in walking, decreased muscle strength and flexibility are usually typical symptoms we see in Parkinson’s. As such, Parkinson’s presents a higher risk of falling. It is important to be mindful of safety concerns, if you have Parkinson’s.
- Mood changes – if you are going through a lot of physical changes and you’re aware of those changes, those changes can often lead to depression. We see depression, social withdrawal and heightened anxiety. It can be very frustrating and embarrassing for someone with Parkinson’s who is dealing with these symptoms and are in a social setting or mealtime. The mood changes can also be seen in the caregiver.
How can therapy help with managing Parkinson’s disease?
Parkinson’s can lead to increased falls and balance impairment, difficulty walking and shuffling feet. These symptoms fall under physical therapy. We can increase muscle tone, strength and coordination. This can help you improve how you function daily, especially with walking and even getting out of a chair. It is so important to strengthen your muscles and regularly move. You don’t want to lose muscle strength and control. Physical therapy can create a good game plan and routine that’s beneficial for you; we don’t want to be unrealistic.
Some people are more motivated than others, and that’s okay. This is true with anything, even outside of Parkinson’s. Some people are more motivated to exercise than others. We want to give you an exercise program you can maintain and is going to be successful for you.
Many times, your daily routine, things like getting up out of a chair, going to the bathroom, doing the laundry and even fixing a meal can become very taxing when you have Parkinson’s, especially as it progresses. Therapy can help improve those activities. We don’t want your daily activities to be stressful and taxing. We want to see you feeling like, “okay, I can make lunch, or I can get in my afternoon activities and not be so exhausted that I can barely eat dinner,” so you can enjoy life.
When you come to therapy, we might pick four or five different activities and have you rate them, whether they’re mild, moderate or severely difficult for you. We then reassess those halfway through the physical therapy session, maybe two weeks into the therapy and then again at the end of the first month to assess if there has been any improvement. We’ve seen a lot of good improvements and coordination with physical therapy for Parkinson’s.
Safety and managing Parkinson’s disease
 We also want to be mindful that we’re being safe. We want to work on balance strategies. Balance becomes greatly impaired with Parkinson’s – including the self-awareness of balance issues. If you’re starting to lose your balance, the realization doesn’t really kick in as quickly for someone with Parkinson’s. This relates again to muscle strengthening. We want to be aware of the muscle strength, but also of that self-awareness and perception of where your body is in space.
We also want to be mindful that we’re being safe. We want to work on balance strategies. Balance becomes greatly impaired with Parkinson’s – including the self-awareness of balance issues. If you’re starting to lose your balance, the realization doesn’t really kick in as quickly for someone with Parkinson’s. This relates again to muscle strengthening. We want to be aware of the muscle strength, but also of that self-awareness and perception of where your body is in space.
This should help you if you start to lose your balance and go backwards so you can step back and right yourself. You would have the strength and awareness to step back and correct your loss of balance versus continuing to teeter backwards and then having an actual fall. This is very important in physical therapy and one we usually focus on with our patients.
The BIG program
Many of you may have heard about the BIG program. The Big program is for Parkinson’s patients, to help them manage Parkinson’s disease. It’s very specific. Allison, my colleague, and I went to New York about three years ago for training in the BIG program.
The BIG program focuses on big movements because with Parkinson’s there’s a lot of rigidity. You start to come inward. Reaching out, walking … there are not a lot of big movements. In Parkinson’s, your steps are small, almost like baby steps or shuffled steps. What we focus on in the BIG program is really big movements, emphasizing your movements, taking big and giant steps. Some residents have even heard us cueing our patients, which might sound funny and exaggerated. We’re trying to cue them into loosening up and becoming more flexible and taking big steps and movements. In the minds of Parkinson’s patients, if we cue them to take big movements, their big movements are more like normal movements. They think they are already moving normally, but in fact the movements are more diminished, rigid and shallower.
If we can get the mind connecting with those movements and thinking, “okay, I’ve got to move big,” but they’re just reaching out to the side for something, that’s really not exaggerated. We don’t go around walking like a soldier, like we practice in physical therapy. But we’re trying to loosen up and improve the coordination and muscle control.
The BIG program, I want to emphasize, is very specific and has a very rigid protocol, which includes four times a week for four weeks in the physical therapy department. You are also doing an exercise program outside of therapy daily. We have seen many good results. We have had several Carroll Lutheran residents who have gone through the program. If you’re interested in it, we can definitely talk to you more about it. We can also connect you with someone who has gone through the program and will discuss it with you.
The BIG program is not for everybody, and that’s okay. We can also do regular exercise programs and customize them for you. I just want to emphasize that it’s a very rigid protocol to follow. Some people are more motivated and that would be fine for them, but it might be a little bit too much for others, and that’s okay. In your initial evaluation, we discuss this and customize the best plan for you.
There are a lot of things we can do with you through the stages of Parkinson’s, and what might work early on might not work within a couple months or years down the road. You might need to come back to therapy and have a refresher course, and that’s okay. We’ve had many residents do that inside and outside of the Parkinson’s program.
What do we need to get you started?
We are here for you and can help you through the stages of Parkinson’s by helping you to manage Parkinson’s disease. We need an order from your doctor to start the process and to call us for an evaluation. You can call Kathy at the outpatient office. The number is 443-605 1009.
We are practicing safety guidelines from the CDC. We’re still wearing masks. We’re cleaning between every resident. I want you to know it’s a safe environment; we’re still maintaining safety and safety awareness on all levels. Please reach out for help.
Our goal is to optimize your functionality and reduce the stress that can come from having Parkinson’s. Let us partner with you to make your life safe and happy.
